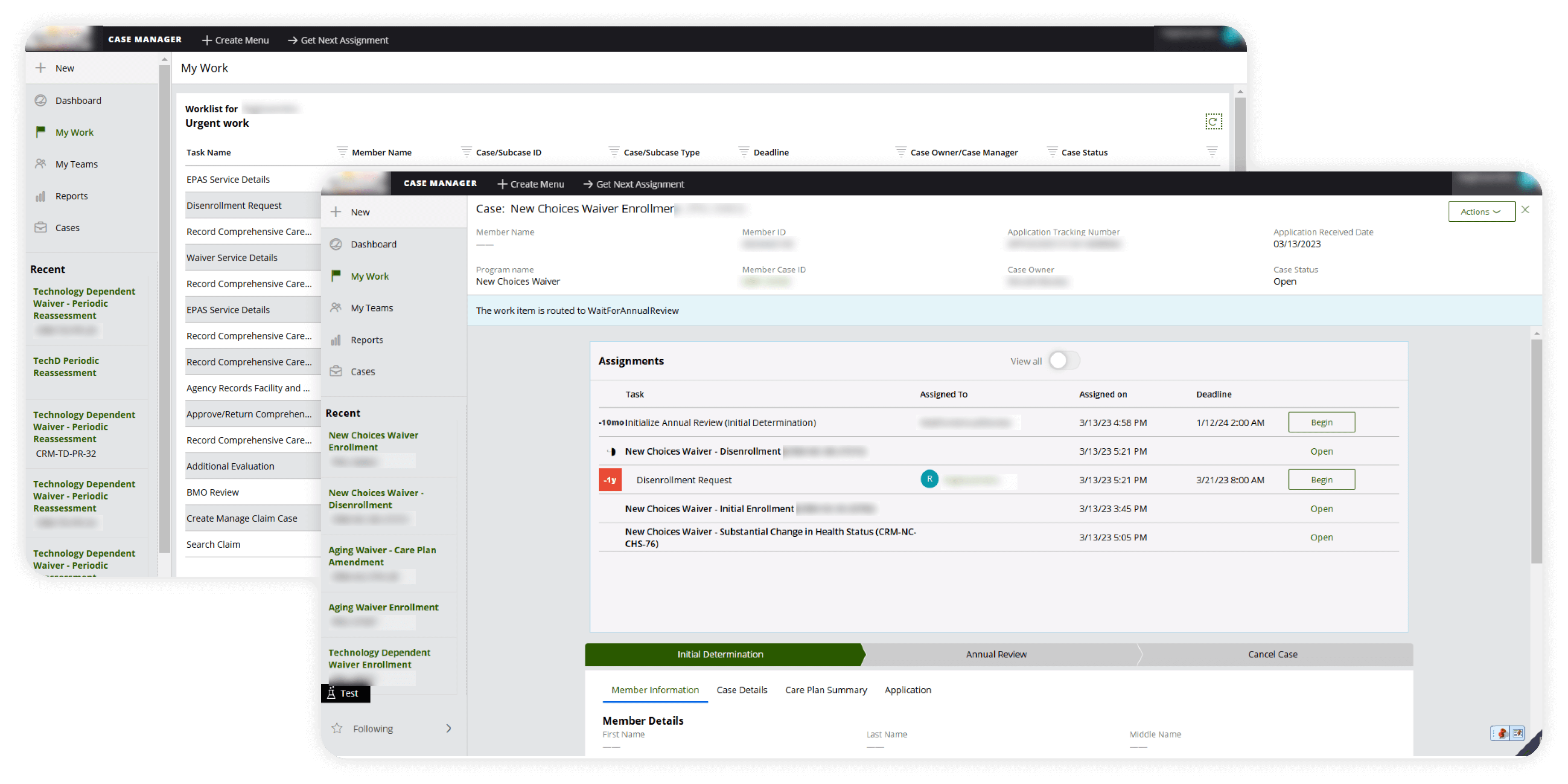
The state government sought to modernize four of its eleven Medicaid Home and Community-Based Services (HCBS) Waiver programs and improve tracking across various case management processes, including claims, complaints, appeals, prior authorizations, and more. They required workspace portals for case managers and case workers to support the multiple roles involved throughout the HCBS program lifecycle, from enrollment to disenrollment. These portals were designed to enable efficient management of diverse case types while adhering to established business processes.